Senior Group Leader Dr. Martin Sprick
Senior Group Leader Prof. Dr. Andreas Trumpp
Metastases are tumor growths that have spread from a primary tumor to distant organs. The chances of cure are much lower if the primary tumor has already formed metastases. In fact, metastization is the main cause of death in cancer patients because the majority of cancer treatments are no longer effective in this late stage of the disease.
Metastases develop when cancer cells detach from the original (primary) tumor and travel via the blood or lymph to other parts of the body, where they settle and multiply. Although current techniques make it possible to detect and quantify tumor cells in the bloodstream, nothing about their biology or function is known. Researchers at Hi-STEM assume that only circulating tumor cells of CSC origin function as metastasis-inducing cancer stem cells (MIC).
The identification of new biomarkers is a major goal of two HI-STEM research groups working under the direction of Dr. Christoph Rösli and Dr. Martin Sprick. Quantitative detection of MICs in the bloodstream and bone marrow of cancer patients could have two major benefits: it could significantly improve the diagnosis of cancer and could make it possible to more quickly assess the results and benefits of treatment. HI-STEM is working together with different departments of Heidelberg University Hospital (Gynecology and Surgery), the National Center for Tumor Diseases (NCT), the Institute of Tumor Biology in Hamburg, and Merck-Serono in Darmstadt to find ways to detect and eliminate metastasis-inducing cancer stem cells.
Our goal is to develop new diagnostic markers that enable the detection and quantification of MICs in the bloodstream of cancer patients. In parallel to this, HI-STEM is working closely with Merck-Serono to develop new drugs capable of achieving the long-term eradication of circulating MICs and established metastases in the near future.
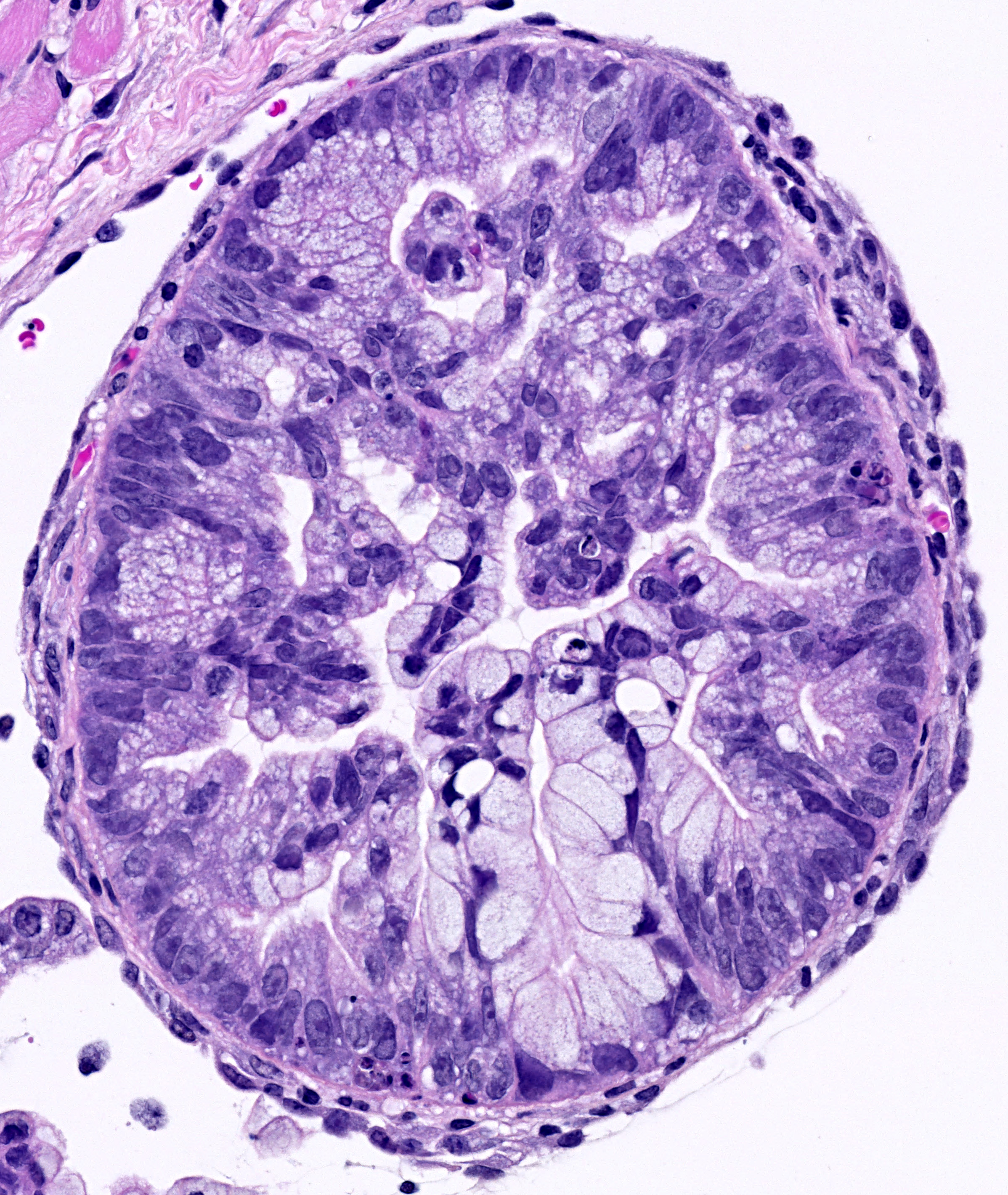
In Pancreatic Cancer we have recently uncovered three novel subclasses of human pancreatic cancer and have developed biomarkers to identify them. Stratification of patients according to the subtypes revealed striking differences in their overall survival. Tumor cells isolated from these patients show differential sensitivity to conventional and targeted therapies. We then identified a novel mechanism used by tumors to display primary and develop secondary resistance against paclitaxel and tyrosine-kinase inhibitors. Pancreatic cancer cells up-regulate CYP3A5, a member of the P450 system, to efficiently metabolize and inactivate these drugs in a cell autonomous manner (Noll et al., Nature Medicine, 2016).
We are currently developing tools to break resistance to commonly used clinical drugs in pancreatic cancer with the goal to improve the efficacy of targeting this devastating disease. Moreover, next generation sequencing and molecular characterization of subtype specific cancer and metastasis stem cells will provide the basis for the generation of novel diagnostic and therapeutic tools to target advanced therapy resistant cancers, including metastasis.
Noll, E.M. et al. 2016. “CYP3A5 Mediates Basal and Acquired Therapy Resistance in Different Subtypes of Pancreatic Ductal Adenocarcinoma.” Nature Medicine 22 (3): 278–87. https://doi.org/10.1038/nm.4038 .